The preservation of meaning:
Around the globe, there’s a growing body of opinion that suggests the most significant technical issue in healthcare[1][2][3] to be solved is the challenge of siloed patient data due to the semantic interoperability issues and the resulting inability to produce a single unified lifelong patient electronic health record (EMR).
At this issue’s core, let’s consider the problem of the “preservation of meaning”[4] across various patient records systems:
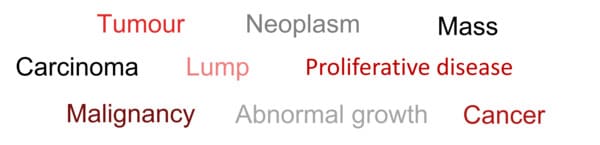
Consider the following words:
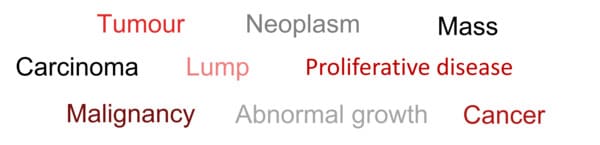
These words could describe what was wrong with a patient suffering from a particular form of cancer. The comments all share a certain commonality of meaning. They’re not exact synonyms, however; some general terms refer to the disease’s main symptom – a lump or mass – without necessarily carrying any implications for diagnosis. There are also differences between the diagnostic terms: carcinoma is a more precise diagnosis than cancer.
These differences in precision and emphasis occur in medical language because they’re general language features. We can communicate effectively using natural language because we bring enormous amounts of background knowledge and an understanding of the context when interpreting words that make up a sentence.
Many communication problems in healthcare occur when the people involved do not share the same background. Issues arise when words are used in computer software without an appropriate context, such as labels that define categories. It is increasingly essential for computerised patient record systems to identify all the patients with a particular condition, say diabetes. Simply searching the records for any word occurrence would probably succeed on most occasions but fail on many others.
Consider a search using the word ‘diabetes’. This would only detect patients whose diagnosis was recorded using this precise word. It would not see patients registered as ‘diabetic’ or ‘NIDDM’ (a common abbreviation for ‘non-insulin-dependent diabetes mellitus). It would, however, include patients whose records contained the words in other contexts, for example, “suspected diabetes,” “worried about diabetes”, or “parents have diabetes”.
The need for comprehensive standards:
Controlled clinical terminologies, or coding systems, have been developed to solve these problems. These include but are not limited to:
- The World Health Organisation - International Classification of Disease (ICD)[5] –ICD11 around 55,000 terms;
- International Health Terminology Standards Development Organisation - Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT)[6] – around 450,000 concepts.
However, neither of the above ontologies covers the entire healthcare requirement. There’s a need for additional vocabularies across the whole healthcare domain,[7][8] which we will consider in greater detail subsequently.
Why is semantic interoperability so important in healthcare? The use of high-quality and comprehensive patient data is essential to delivering an efficient and effective healthcare service, minimising costs, and reducing errors which lead to death and severe injury,[9] with USA-based research estimating over 100,000 deaths each year from identity errors or “wrong patient errors” in the United States[10], duplication of effort, improving outcomes and using limited clinical resources more optimally[11] facilitating the much-promised but rarely delivered benefits of eHealth.
Healthcare is one of the most complex sectors in our economy. Therefore, the ability to generate comprehensive and accurate patient data is a fundamental and essential requirement. It’s been over half a century since the seminal paper on EHR[12] was published in the New England Journal of Medicine that outlined the fundamental requirements for a unified lifelong patient EHR. Unfortunately, to date, no nation has yet managed to deliver a single unified lifelong EHR after a global expenditure on such systems of US$ 100’s billion.
With healthcare systems around the world challenged by ageing populations increasing demand, rising expectations, and insufficient clinical staff and allied professionals thus face the question of fiscal sustainability. Therefore, we must harvest the much-needed benefits EHRs should deliver, improving outcomes, reducing costs, and supporting more preventative medicine and integrated care systems via comprehensive and regulated standards.
Suggested areas requiring global standard terminology:
After half a century of this EHR problem’s existence, it’s time for it to be resolved. According to Albert Einstein, to keep doing the same thing and expecting a different result is the definition of insanity. The resolution of the semantic interoperability issue in healthcare is fundamental to an efficient and effective Integrated Care System (ICS) and a move to a more preventative form of healthcare. Let’s look at some key areas that need our attention:
- Pathology/lab tests and diagnostic imaging coding, including naming conventions, reference ranges and units of measure[13]. Reducing unwarranted variation in diagnostic testing and facilitating semantic interoperability of the resulting data
- Dictionary of medicines and devices (dm+d), a global standard dictionary containing unique identifiers and associated textual descriptions for medicines and medical devices[14] applied consistently
- Genomics utilising the EHR to present information which support the use of genomic medicine in clinical care to improve outcomes represents a tremendous opportunity. However, numerous barriers prevent the effective use of the EMR for this purpose[15]. To fully realise the value, it’s critical to place credible information in the hands of clinicians in time to support clinical decision-making
- Medical device approval processes are complex and time-consuming, with differing standards in various geographical zones[16]. There is a need for device manufacturers to have a speedy single global approval process to facilitate rapid technological development and associated healthcare and patients benefit
And subsequently:
- Clinical “best practise”, a single consistent source of truth that means doctors and other healthcare professionals can get to the exact chunk of knowledge in an easily assimilated format they need at their fingertips to provide a smooth clinical workflow[17]
- Individualised care pathways [18] - more people than ever are living with long-term conditions, including physical and mental health problems. As a result, there’s been a drive towards providing people with long-term, personalised care plans. Personalised care planning standards will help enable people to manage their own care, with the support of a wide range of services, including primary healthcare, hospitals, occupational therapy and social care[19]
- Artificial Intelligence (AI) standards including “clinical alerts” and “patient segmentation on risk”,[20] minimising false positives and false negatives
- Computerised physician order entry (CPOE) – order sets [21]
Implementation:
It’s essential to recognise that implementing these standards is complex[22] and can take a considerable amount of time and effort. For example, NHS England has spent two decades implementing SNOMED CT across its entire domain and still has a significant way to go, though it did set a deadline for April 2020[23]. It’s essential therefore to ensure access to competent implementation and training resources. It’s also important to understand that clinical terminologies are dynamic and subject to change. We need to provide such changes are implemented promptly and consistently across the entire operational domain and EMR systems.
Regulation:
There’s suggestion that the proposed comprehensive terminology standards should be mandatory and supported by appropriate law. Perhaps the most encouraging of several recent developments is that of the recently published (May 2022) Proposal for the Regulation of the European Parliament and The Council – on the European Health Data Space, which comprises an annexe addressing the following:
- Annexe I - Main Characteristics of Electronic Health Data Categories;
- Annexe II - Essential Requirements for EHR Systems and Products Claiming Interoperability with EHR Systems;
- Annexe III - Technical Documentation;
- Annexe IV - EU Declaration of Conformity.
Who might be involved in developing comprehensive clinical standards?
Undoubtedly now is the time for various healthcare ecosystems to come together and lead to assist in developing and implementing appropriate standards. This would include, I suggest, such organisations as, but not limited to, the World Health Organisation, which would facilitate the correct constitutional setting and BSI, which operates in over 190 countries around the globe and has a wealth of experience in standards development implementation and training, EMR vendors, medical and consumer technology manufacturers, cloud providers, software platform providers dealing with patient and healthcare data alongside policy makers, healthcare providers and healthcare insurance companies. There are significant potential benefits for all stakeholders.
Benefits:
There’s a global opportunity to:
- accelerate innovation
- reduce costs
- reduce errors
- improve patient outcomes
- make more optimal use of scarce clinical human resources
- facilitate the requirements of EHRs for integrated care.
Suppliers and manufacturers to deliver healthcare without borders in a truly global market and assist developing nations in avoiding the legacy issues of the West and providing affordable high-quality healthcare to their citizens. The geopolitical element of this transformation is undoubtedly considerable.
Should we not develop these comprehensive terminology standards, it’s unlikely that eHealth and EMRs can progress significantly and deliver the considerable available benefits.
The above proposal would significantly deliver major benefits significant to all involved in healthcare, not just the patient going forward. However, there remains the major challenge of using legacy data and the semantic challenges that exist. I’ll address this in a future blog.
Endnotes:
[1] Proposal for the Regulation of the European Parliament and The Council – on the European Health Data Space - https://health.ec.europa.eu/publications/proposal-regulation-european-health-data-space_en
[2] Oracle thinks it can fix healthcare’s biggest tech issue - https://www.theverge.com/2022/6/10/23162503/oracle-cerner-health-records-data-interoperability
[3] The World's First Cross-Border Digital Health Framework Programme - shared interoperability standards across Sweden, Denmark, Norway, Finland and Iceland - https://norddec.org/
[4] From Patient Data to Medical Knowledge - The Principles and Practice of Health Informatics – by Prof Paul Taylor - Professor of Health Informatics at UCL - ISBN:9780470994696
[5] The World Health Organisation - International Classification of Disease - https://www.who.int/standards/classifications/classification-of-diseases
[6] International Health Terminology Standards Development Organisation - Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT)- https://www.snomed.org/
[7] fdb –Ian Arrowsmith shares his thoughts on the new draft document from NHS England/Improvement Transformation Directorate - https://www.fdbhealth.co.uk/insights/blog-article/2022-07-26-ian-arrowsmith-comments-on-how-standards-will-support-interoperability
[8] The Faculty Of Clinical Informatics - NHS Transformation Directorate Standards & Interoperability programme Strategy Review & Consultation - https://facultyofclinicalinformatics.org.uk/blog/faculty-of-clinical-informatics-news-1/post/how-standards-will-support-interoperability-90
[9] Health Data Management - Avoiding healthcare interoperability ‘train wrecks’ - https://www.healthdatamanagement.com/articles/avoiding-healthcare-interoperability-train-wrecks?utm_campaign=HDM%20Group%20Newsletters&utm_medium=email&_hsmi=211200577&_hsenc=p2ANqtz-9ZbBeNnEXCGOkoFlz6_30Lui_iCOysxbrzDflGIJU_H3dyQYnSU_bztD_7g-z14M8h3TWA6M0pClZyDm1r1FCp6C7_uQ&utm_content=211200577&utm_source=hs_email
[10] The Online Research Journal in Health Information Management.-.Why Patient Matching Is a Challenge: Research on Master Patient Index (MPI) Data Discrepancies in Key Identifying Fields - - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4832129/
[11] The European Institute for Innovation through Health Data (i~HD) - Data quality, a dynamic complexity - https://www.i-hd.eu/data-quality-a-dynamic-complexity/
[12] New England Journal of Medicine - Medical Records that Guide and Teach – by Dr Larry Weed - Pub March 1968 https://www.nejm.org/doi/10.1056/NEJM196803142781105?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
[13] NHS England - The atlas of variation in diagnostics – by Sir Muir Gray - https://fingertips.phe.org.uk/documents/Atlas_2013%20Diagnostics.pdf
[14] NHS England - a dictionary containing unique identifiers and associated textual descriptions for medicines and medical devices - https://qualitysafety.bmj.com/content/28/12/987; https://www.datadictionary.nhs.uk/supporting_information/nhs_dictionary_of_medicines_and_devices.html
[15] Genomic Information for Clinicians in the Electronic Health Record: Lessons Learned from the Clinical Genome Resource Project and the Electronic Medical Records and Genomics Network - https://www.frontiersin.org/articles/10.3389/fgene.2019.01059/full
[16] TWI - WHAT IS THE MEDICAL DEVICE DEVELOPMENT PROCESS? (INCLUDES STAGES) - https://www.twi-global.com/technical-knowledge/faqs/what-is-the-medical-device-development-process
[17] BMJ Best Practice - Clinical decision support: integration into electronic health records - https://bestpractice.bmj.com/info/clinical-decision-support-integration-into-electronic-health-records/
[18] Professional Record Standards Body (PRSB) - Personalised care and support plan - https://theprsb.org/standards/personalisedcareandsupportplan/
[19] NHS England – Universal Personalised Care - Implementing the Comprehensive Model - https://www.england.nhs.uk/wp-content/uploads/2019/01/universal-personalised-care.pdf
[20] International Journal of Medical Informatics - Best practices for preventing malfunctions in rule-based clinical decision support alerts and reminders - https://www.sciencedirect.com/science/article/abs/pii/S1386505618305173
[21] BMJ Quality & Safety - When order sets do not align with clinician workflow: assessing practice patterns in the electronic health record - https://qualitysafety.bmj.com/content/28/12/987
[22] Clinical Terminology: Why is it so hard? – by Alan L. Rector - https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.101.6701&rep=rep1&type=pdf#:~:text=The%20first%20reason%20clinical%20terminology,users%20is%20very%20large%20indeed
[23] NHS England - SNOMED CT - https://www.england.nhs.uk/digitaltechnology/digital-primary-care/snomed-ct/